Prevent claim rejection – No more spending countless time on the phone chasing insurance companies and then mailing out invoices for each patient. Within 20 seconds, verify patient insurance coverage and eligibility electronically AND receive patient payment at point of care.
Prevent claim rejection – No more spending countless time on the phone chasing insurance companies and then mailing out invoices for each patient. Within 20 seconds, verify patient insurance coverage and eligibility electronically AND receive patient payment at point of care.
Arrange or secure payments in recurring automated format or by capturing a payment method on file for post adjudication collection thus eliminating the need for invoices or collection efforts later.
Immediate Reimbursement – Print an EOB at POC in line item format so patient can see what they owe and why, this allows collection to be non confrontational and routine.
And…Patient signs the EOB acknowledging that they owe the balance, eliminating confusion when they later receive statements.
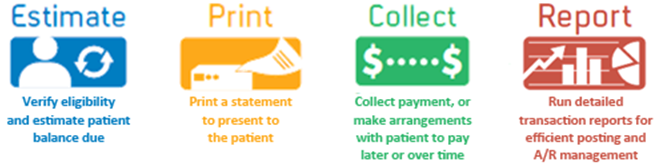
How RevMax Plus Works
Instantly verify patients’ insurance coverage, and eligibility to obtain detailed benefit information, and estimate patient balances owed based on your billed charges and payer contracted rates.
Establish co-pay, coinsurance, and remaining deductible amounts and then present a patient-friendly statement to patients to review charges and ask how they would like to pay. Patient friendly statement helps office staff set and manage patient expectations.
Collect payment from patients by cash, check, credit/debit card or ACH – at the point of care, OR after insurance has paid use card on file with pre authorization signature from patient, collecting monthly installments over time using the schedule payments feature. Patients can even pay online using the patient payment portal.
Use the comprehensive reporting tools to simplify daily reconciliation, end of day closing, and improve tracking of payments activity by location, department, payment method, user. Exportable transaction file enables automatic electronic posting with integration to PM system.
Earn a Return on Investment
*Improve Cash Flow
–Receive patient payments 30-120 days sooner with less bad debt
*Increase Staff Efficiency
–Reduce amount of time verifying eligibility & determining what patient owes
–One system to accept and record any form of payment from patients
–Eliminate manual patient payment posting & ease reconciliation via integration with PM system
*Decrease Billing and Collection Costs
–Collect more from patients at point of care by estimating what’s owed
–Obtain authorization to charge patient’s stored card or ACH funds from bank account eliminating the need to sendbilling statements
*Provide Patient Payment Options
–Multiple ways for patients to pay – cash, check, ACH, credit/debit or online
*Deliver Patient Convenience and Satisfaction
–Improve patient experience by communicating what’s owed at Point of Care
–Let patients in financial difficulty pay off larger balances over time
–Patients can use the convenience of paying bills online
Provide Better Patient Communications
Through Us……
We will provide you with the following to help communicate the message to your patients:
– In-office signage
– Scripts for office staff
– Patient brochures and letters customized to your practice
– Patient notification statements upon payment
Seeing Is Believing!
 This is a snapshot of our healthcare practices seeing drastic revenue increases. Some practices see as much as 2 – 4 times their revenue in just a couple of months.
This is a snapshot of our healthcare practices seeing drastic revenue increases. Some practices see as much as 2 – 4 times their revenue in just a couple of months.
For more information on the standalone payment gateway, Revenue Mazimizer, please feel free to call us at: 800-288-1358 or email us.